NewYork-Presbyterian Lawrence Hospital
SW: Give us a sense of the impact of COVID-19 on you and the ER staff from when people first started
coming to the ER, and then as it grew and did not let up.
AA: Since January of 2019 when I joined the team here at NewYork-Presbyterian Lawrence we had
several emergency situations including the 1 Garret Place fire and the episode where the hospital was in
emergency lockdown. So, while we drill and prepare for different types of emergencies like highway
accidents etc., COVID-19 presented a whole new set of challenges including the fact that it has endured
over a couple of months. Here is where our connection to NewYork-Presbyterian Hospital and Columbia

Emergency Medicine where I am on the faculty came into play. We were able to tap into a whole team of disaster preparedness
specialists who guided us through process, training and resources to manage something on this scale. One example is that we were
faced with having to rapidly segregate COVID patients from non-COVID patients, and because of our strong connection to Columbia,
we were able to secure special self-contained isolation tents for each patient which meant we did not have to wait for time consuming
changes in the emergency room layout and were able to maintain continuity.
As far as treatment is concerned, we started out just screening people who had travel history but by the early part of March
we saw that the virus presented in a lot of different squirrelly ways. Then we realized it was in the community and shifted and started
treating everyone who came through the emergency room as potentially having the virus. We isolated them and issued the masks to
everyone both patients and staff and implemented other PPE protocols. Even today, we still maintain high levels of PPE including
masks and related equipment. However, we now try and geo-locate non-COVID patients in a separate area of the emergency room.
Also, when the patient comes in from our EMS partners, they do the initial screening and prep the patient, and we know what
department they should be sent to and their likely COVID status. If you come in as a walk-in, you will be met by a screener who will
supply you with a mask and ask you a series of questions to help determine your status. Also, it’s important to communicate that we
have created pathways to handle all types of non-COVID emergency cases including cardiac events, acute illness, accidents, etc. and
the community should feel confident we are here to help them. In addition, I want to acknowledge our partners at Empress Ambulance
who also were hit hard and had to bring in extra equipment and personnel to manage the overwhelming demand. Our local nursing
homes and rehabilitation facilities were equally challenged and had to scramble for resources and did their very best to care for their
patients.
SW: On a personal level how do you manage the challenges of being a physician on call in the ER facing a myriad of COVID and non
-COVID patients coming through the ER day and night and then going home to your family worried about passing the infection? Or,
just managing the stress of coping with this outbreak and the endless struggle to help your patients but still be available to your family
and keeping them safe?
AA: On a personal level, I am kind of lucky that my wife is a physician so she was in the thick of it herself and was very
understanding, but the truth of it is that healthcare people across the country and across the globe have been dealing with a lot of
stress when it comes to the concern of exposing family members. We know a lot more about the transmission of the virus and how to
protect ourselves than in February. Now the medical community is beginning to accept the fact that this virus is causing a lot of strain
on healthcare workers, and some are struggling with those effects. To the credit of the hospital there are just a wealth of resources
within the hospital for folks who are having logistics issues with childcare or need financial support. The hospital has also provided
support for mental health services. It is a stigma and physicians in particular are the last to admit they are suffering with mental health
issues, but we are human like everyone else and these were traumatic weeks and months and I think that giving a nod to the
enterprise, the hospital has been incredibly generous in providing this type of support to all of our personnel.
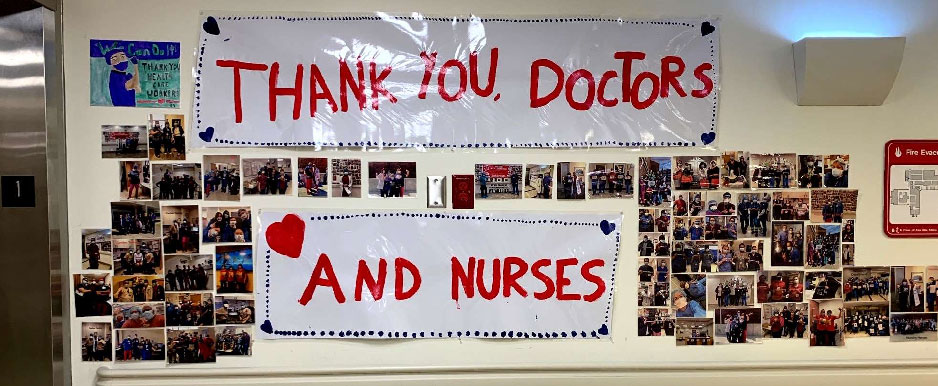
SW: I asked Dr. Amaranto his feelings about the community response in support of the healthcare heroes comprised of the staff of
The views and opinions posted or expressed on this website on any message board, chat area, bulletin board, forum, or any other interactive area are those of the authors and do not purport to reflect the opinions, views or positions of the Armour Villa Neighborhood Association® or its Board of Directors.